Raj C. Dedhia, MD, MSCR, and David Kent, MD, are otolaryngologists board-certified in sleep medicine and recipients of the AASM Foundation American Board of Sleep Medicine Junior Faculty Grant. Learn about what made them pursue a career as physician scientists, their research interests and achievements, and opportunities for otolaryngologists to address patient care gaps through sleep research.
Development of an effective alternative surgical therapy for obstructive sleep apnea
David Kent, MD, is an assistant professor of otolaryngology, head and neck surgery and director of sleep surgery at Vanderbilt University Medical Center. His research interests lie in the neurophysiology of the upper airway, with a focus on mechanisms for control of breathing in obstructive sleep apnea (OSA) and their application towards novel OSA treatments.
“As a surgeon, it’s challenging to examine a patient with severe OSA who is breathing quite comfortably while awake in the exam chair,” said Kent. “The dichotomy between the effortless breathing of wakefulness and the struggle for air during sleep is fascinating to me considering that the underlying anatomy remains the same.”
While continuous positive airway pressure (CPAP) is well-recognized as an efficacious therapy for OSA, its effectiveness is compromised by frequent patient intolerance to therapy. For some patients struggling with CPAP, surgery may be a more effective treatment option, but balancing surgical morbidity against efficacy can be challenging. This conundrum motivated Kent to pursue a physician scientist career with the goal of finding therapy options for OSA that are highly successful while also highly acceptable to patients.

Kent (left) and his surgical research team
In 2019, Kent was awarded the American Board of Sleep Medicine Junior Faculty Grant for a project titled, Ansa Cervicalis Neurostimulation in Obstructive Sleep Apnea.
“Ansa cervicalis stimulation (ACS) was recently proposed as a novel possible neurostimulation mechanism for maintaining airway patency during sleep. Most OSA surgeries are designed to either remove obstructing tissues, or to stretch the airway anteriorly to reduce collapsibility,” explained Kent. “ACS instead stretches the airway inferiorly, much the same that CPAP does when it fills the lungs and increases tracheal traction on the airway.”
The goal of this ongoing project is to assess the effect size of ACS during sedated sleep among patients with different airway phenotypes.
“The support of the American Board of Sleep Medicine Junior Faculty Grant created a wonderful opportunity for us to dramatically enhance our scientific protocol for evaluating ACS,” said Kent. “We have transitioned from coarse assessments of peak inspiratory flow changes with ACS to a highly refined protocol simultaneously capturing changes in airflow and cross-sectional areas across a variety of airway states, which will allow us to better quantify how ACS works, how well it works, and who it works for.”
Data collected from Kent’s project funded by the American Board of Sleep Medicine Junior Faculty Grant directly supported his recently funded National Heart, Lung, and Blood Institute (NHLBI) R01 grant, The Effect of Ansa Cervicalis Neurostimulation on Airway Patency in Obstructive Sleep Apnea. The R01 grant will enable Kent and his research team to scale up their current physiologic experiment efforts, including assessments of ACS in natural sleep, which was all made possible through the equipment and support provided by the AASM Foundation grant.
Elucidating the cardiovascular effects from surgical therapy for OSA
Raj C. Dedhia, MD, MSCR, is an associate professor of otorhinolaryngology: head and neck surgery and medicine in the division of sleep medicine. He is also director of the division of sleep surgery and CPAP alternatives clinic at the University of Pennsylvania Perelman School of Medicine. His research interests are in better understanding both the mechanism and consequences of OSA in the treated and untreated states.
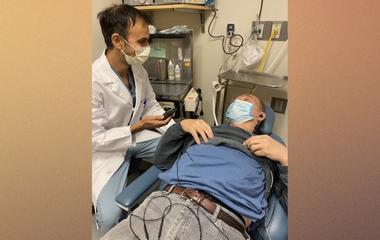
Dedhia (left) and his study participant
“I am fascinated by sleep-disordered breathing. Each airway seems to have both common and unique pathophysiology,” said Dedhia. “In addition, the downstream consequences of this disease are remarkably heterogeneous.”
OSA is known to be associated with an increased incidence and progression of different types of cardiovascular disease such as heart failure, stroke, and coronary heart disease. In patients with OSA who are CPAP-intolerant, surgery can be an effective treatment which personalizes patient care and potentially improves long-term cardiovascular effects.
This led to Dedhia’s 2017 American Board of Sleep Medicine Junior Faculty Grant for a project titled, Hypoglossal Nerve Stimulation on Vascular Function In Patients With Obstructive Sleep Apnea. The goal of this project is to understand the effect of hypoglossal nerve stimulation on intermediate markers of cardiovascular risk. To date, the project has shown that the cardiovascular effects of OSA treatment with hypoglossal nerve stimulation are relatively subtle, which is similar to findings in CPAP trials. In addition to these results, the project has helped Dedhia develop a research team, understand key factors in patient recruitment, collaborate with cardiology researchers and adapt the performance of patient-level research in the midst of a pandemic.
“The American Board of Sleep Medicine Junior Faculty Grant has jumpstarted my research career,” said Dedhia. “In combination with an American Heart Association Career Development Award, I was able to add other important outcome measures, such as 24-hour blood pressure, to this randomized, sham-controlled, crossover study. The results will be forthcoming and likely to have a meaningful impact on our understanding of cardiovascular risk reduction with OSA therapy.”
In 2019, Dedhia, in collaboration with co-principal investigator, Alan Schwartz, MD, received an R01 grant from the NHLBI, Lingual muscle control of upper airway patency in obstructive sleep apnea, to study the mechanism of hypoglossal nerve stimulation on upper airway patency. This research has the potential for Dedhia and Schwartz to develop novel strategies for targeting specific defects in the control of pharyngeal patency by activating specific lingual muscles that relieve pharyngeal obstruction during sleep.
Untapped opportunities in otolaryngology and sleep medicine research
With some patients with OSA inadequately using CPAP, both patients and providers are seeking alternative treatment options. Dedhia and Kent agree that otolaryngology providers have the potential to positively impact the care and outcomes for patients with OSA, as a specialty that provides various opportunities for research.
“The world of research is a sleep otolaryngologist’s oyster. The opportunities are infinite,” said Dedhia. “In general, however, they come in three areas: patient selection criteria, surgical techniques, and patient outcomes. Each of these areas remain severely underdeveloped with a corresponding need for rigorous study.”
“Otolaryngologists are well-positioned for deep explorations of the neurophysiology and intricate anatomy of the upper airway as it relates to OSA,” Kent added. “While surgery can be quite effective in appropriately selected patients, there is a dearth of data regarding accurate procedural selection, the long-term efficacy of surgery for OSA patients, and the effects of surgery (or lack thereof) on associated comorbid diseases.”
The American Academy of Sleep Medicine recently published a systematic review on the referral of adults with OSA for surgical consultation, which provides future research directions for otolaryngology-sleep researchers to further study and develop efficacious and effective alternative treatments for patients with OSA, which Dedhia and Kent are actively working to address.






